Thoracic Disc Herniation
Written By: Stephen Byrne Neurosurgeon and Complex Spine Surgeon
Most of the degenerative spinal pathology that we see as specialists as well as in primary care affects the lumbar or cervical spine. This is interesting as the thoracic spine contains a similar number of intervertebral discs and facet joints than the rest of the spine put together. However, the relative immobility of the thoracic region due to the rib cage limits motion-dependent degenerative processes such that most spinal surgeons would really only operate on thoracic disc herniations once or twice over a several year period.
Recently I saw a 52 year old lady with a history of progressive gait disturbance, falls and chest wall pain. She had also recently begun to mobilise with a stick. Neurologically, I noted that she had a Brown-Sequard syndrome (with motor weakness and loss of proprioception and vibrations sense affecting one leg and loss of pain and temperature sensation affecting her contralateral leg). Her CT and MRI scan demonstrated a central and paracentral thoracic disc bulge compressing the spinal cord and a thoracic nerve root.
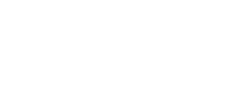
Figures 1 and 2
Sagittal and axial T2 MRI images demonstrating a paracentral T10/11 disc prolapse compressing the spinal cord
Due to the progressive and emergent nature of her presentation and after a frank discussion of the risks and benefits of surgery versus non-operative care, I recommended surgical decompression of the spinal cord. My preferred approach for decompressing the spinal cord due to a disc herniation is via a thoracotomy as this means that absolutely no retraction is placed on the spinal cord as the surgeon can directly work on anteriorly located pathology rather than passing instruments from behind to in front of the spinal cord. The patient subsequently underwent a left sided thoracotomy, removal of the head of the 11th rib and partial T10/11 vertebrectomy and discectomy. She spent a couple of days in HDU as pain control was challenging for her before being discharged home. At recent follow-up, both her chest wall pain and walking difficulties have significantly improved.

Figures 3 and 4
Coronal and sagittal CT images showing the extent of bony resection at T10/11 to perform a thoracic discectomy via a thoracotomy
Thoracic disc pearls
- Many patients (up to around a third) have asymptomatic disc protrusions that, while impressive on imaging, do not require surgery.
- Usually occur below T8 as the thoracic spine becomes ‘transitional’ and the degree of segmental motion increases.
- Most thoracic disc prolapses are calcified making surgery more difficult.
- Different approaches are possible to remove thoracic discs for cord compression but a thoracotomy is associated with the lowest risk of neurological injury.